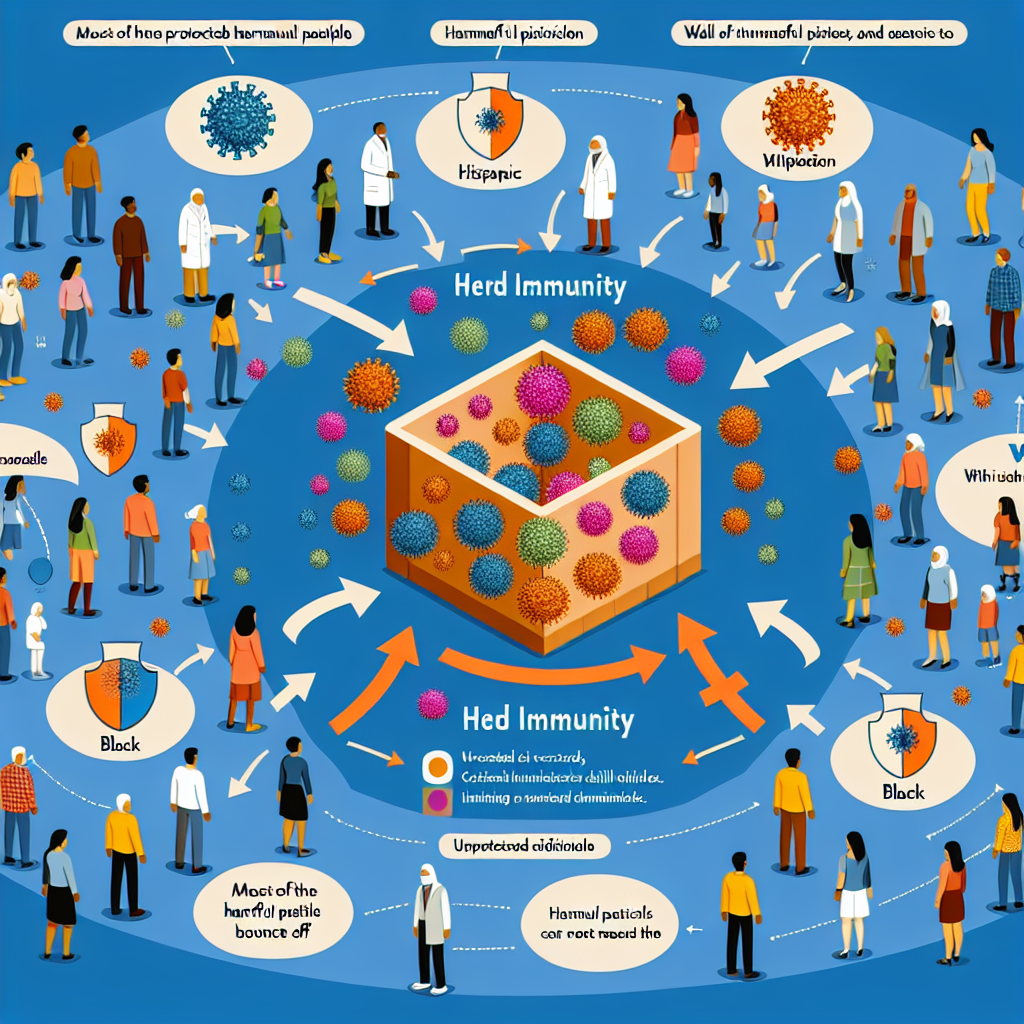
How does herd immunity work?
Herd immunity is a crucial concept in public health that plays a significant role in controlling infectious diseases. It refers to the protection of a population from a disease when a sufficient proportion of individuals are immune, either through vaccination or previous infections. This phenomenon not only safeguards those who are vaccinated but also helps protect individuals who cannot be vaccinated due to medical conditions or age. Understanding how herd immunity works, its reliance on vaccination, and its implications for disease control strategies is essential in combating outbreaks and ensuring community health.
Understanding the Concept of Herd Immunity in Public Health
Herd immunity occurs when a large portion of a community becomes immune to a specific disease, making its spread unlikely. When enough people are immune, either through vaccination or natural infection, the entire population gains some level of protection, as the virus or bacteria has fewer opportunities to spread. This concept is especially vital when considering vulnerable populations, such as infants, elderly individuals, and those with compromised immune systems, who may not be able to receive vaccinations or mount an effective immune response.
The threshold for achieving herd immunity varies depending on the disease in question. For instance, diseases like measles require about 95% of the population to be immune to achieve herd immunity, while for others, such as polio, the threshold may be lower. The ability to contain outbreaks through herd immunity is a testament to the collective responsibility of communities to engage in preventive health measures. As more individuals are vaccinated, the likelihood of outbreaks decreases, ensuring a safer environment for everyone.
In summary, herd immunity is not just an individual health measure but a community health strategy. It transcends personal choices regarding vaccination and emphasizes the interconnectedness of population health. Understanding this concept allows public health officials to develop effective strategies to combat outbreaks and promote widespread vaccination initiatives that benefit society as a whole.
The Role of Vaccination in Achieving Herd Immunity
Vaccination is the most effective way to achieve herd immunity. Vaccines stimulate the immune system to recognize and combat pathogens without the individual suffering from the disease itself. By significantly reducing the number of susceptible hosts in a population, vaccinations lower the chance of disease transmission. This makes it significantly harder for diseases to spread, ultimately protecting those who cannot be vaccinated.
Public health campaigns have emphasized the importance of routine vaccinations for children and vulnerable populations, advocating for the use of vaccines to create a healthier community. For instance, the CDC provides guidelines for vaccination schedules that aim to maximize herd immunity. Vaccination not only protects the vaccinated individuals but also contributes to the overall decline in disease prevalence within the community, which benefits everyone.
Furthermore, vaccination plays a crucial role in eradicating diseases. The eradication of smallpox in 1980 serves as a prime example of how widespread vaccination can lead to herd immunity and ultimately eliminate a disease from the human population. Continued efforts to vaccinate against diseases such as measles, mumps, and rubella are essential to maintain herd immunity and prevent resurgences in disease outbreaks. By prioritizing vaccination, communities can work together to protect the most vulnerable and promote public health.
How Infection Rates Affect Herd Immunity Thresholds
The level of herd immunity required to protect a community is influenced by the infection rate of a disease, which is often measured by the basic reproduction number (R0). The R0 value indicates how many people, on average, an infected person will transmit the disease to in a fully susceptible population. Diseases with a higher R0 require a larger percentage of the population to be immune in order to achieve herd immunity. For example, the R0 of measles is estimated to be between 12 and 18, necessitating a herd immunity threshold of about 95%.
In contrast, diseases with a lower R0 value, such as influenza, may require less than 80% of the population to be immune to achieve herd immunity. This variability highlights the importance of understanding both the transmissibility of a disease and the population’s vaccination coverage. As infection rates change and new variants emerge, public health officials may need to reassess herd immunity thresholds and vaccination strategies in response.
Additionally, factors such as population density, social behavior, and public health infrastructure can impact infection rates and herd immunity. For example, highly interconnected populations in urban areas may experience faster disease transmission, necessitating higher vaccination rates to achieve herd immunity. Continuous monitoring of infection rates and adapting vaccination campaigns are crucial for maintaining herd immunity and preventing outbreaks. It is essential for communities to remain vigilant and responsive to the changing landscape of infectious diseases.
Implications of Herd Immunity for Disease Control Strategies
The concept of herd immunity has significant implications for disease control strategies. It guides public health officials in determining vaccination policies, prioritizing populations for vaccination, and allocating resources. When a community achieves herd immunity, the risk of outbreaks diminishes, leading to fewer cases, hospitalizations, and deaths. This is particularly important in strategic planning for diseases that can have severe health consequences, such as pertussis or COVID-19.
Moreover, herd immunity can influence public perceptions of vaccination. When individuals observe low infection rates due to high vaccination coverage, they may feel less compelled to get vaccinated, leading to complacency. This phenomenon, known as “vaccine hesitancy,” can threaten herd immunity as more individuals remain unvaccinated, increasing the risk of outbreaks. Public health campaigns must therefore continue to emphasize the importance of vaccination and herd immunity to ensure community protection.
Lastly, the ongoing challenges posed by misinformation and vaccine hesitancy highlight the need for robust education and outreach programs. Involving community leaders and healthcare providers in promoting vaccination can help address concerns and reinforce the importance of herd immunity. By fostering a culture of understanding and support for vaccination, communities can enhance their resilience against infectious diseases and protect the health of their members.
In conclusion, herd immunity is a fundamental principle in public health that emphasizes the collective responsibility of communities to protect vulnerable individuals from infectious diseases. The role of vaccination in achieving herd immunity is paramount, and understanding how infection rates affect the necessary thresholds for immunity is crucial for effective disease control strategies. As we navigate the complexities of public health, fostering awareness and promoting vaccination is essential for maintaining herd immunity and ensuring a healthier future for all. For more information on vaccination and public health initiatives, please refer to the World Health Organization and the National Institutes of Health.
Top hand sanitizers for virus protectionSeasonal flu vaccine effectivenessLatest research on virus transmissionRelevant LinkRelevant LinkRelevant Link